Imagine a virus spreading quietly, yet its impact felt strongly in hospitals and among vulnerable populations. Human Metapneumovirus (hMPV) is one such virus, often under the radar but potentially serious. In this article, we will look deeply into what hMPV is, its origins, how it spreads, and the strategies doctors use to combat it.
What is hMPV?
hMPV is a respiratory virus that primarily affects the lungs and airways. First identified in 2001 by researchers in the Netherlands, the virus was isolated from respiratory secretions of young children. Retrospective studies, however, suggest that hMPV has been silently circulating in human populations for at least 50 years.
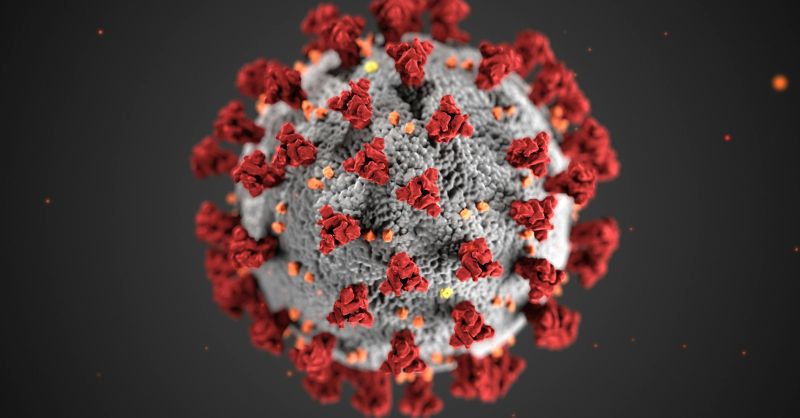
It belongs to the Paramyxoviridae family, closely related to respiratory syncytial virus (RSV). Globally, hMPV is detected in approximately 3%–10% of hospitalizations of children under five with acute lower respiratory tract infections. This makes it a significant cause of respiratory illnesses, particularly in young children, the elderly, and immunocompromised individuals.
How does hMPV attack?
hMPV spreads through respiratory droplets from coughing, sneezing, or close contact. Once inhaled, the virus targets the epithelial cells lining the respiratory tract, causing symptoms like coughing, wheezing, fever, and nasal congestion. In severe cases, it can lead to pneumonia or bronchiolitis, requiring hospitalization. Recent data from China indicates a surge in hMPV cases, especially among children under 14, leading to overcrowded hospitals.
Medications and treatments
Currently, there are no specific antiviral drugs for hMPV. Treatment focuses on managing symptoms and providing supportive care. For mild cases, rest, hydration, and over-the-counter medications suffice. Severe cases may require oxygen therapy, nebulizers, or even mechanical ventilation. Research is ongoing to develop targeted treatments and vaccines to mitigate the virus’s impact.
Is hMPV worse than COVID-19?
While both hMPV and COVID-19 cause respiratory issues, their impact differs. COVID-19 has a broader range of symptoms and a higher potential for severe outcomes and long-term complications. However, hMPV poses a significant risk to specific groups, particularly young children and the elderly. Unlike COVID-19, hMPV lacks widespread awareness and targeted vaccines, making prevention more challenging. The COVID-19 pandemic has heightened global vigilance toward respiratory viruses, but hMPV remains a persistent concern.
Where did hMPV originate?
hMPV was first identified in the Netherlands, but its genetic similarity to avian metapneumovirus indicates a possible zoonotic origin. Retrospective studies suggest that the virus had been present for decades before its discovery. hMPV infections occur globally, with seasonal peaks in late winter and early spring, similar to influenza. Its presence has been particularly notable in regions with cold climates, aligning with other seasonal respiratory viruses.
The lifecycle of hMPV
The virus begins its lifecycle by binding to host cells in the respiratory tract, entering through endocytosis. Inside the cell, it releases its RNA, hijacking the host’s machinery to replicate and produce viral proteins. New virions are assembled and released to infect neighboring cells, perpetuating the cycle of infection and contributing to its rapid spread within communities.
Who should be concerned about hMPV?
While hMPV can affect anyone, certain groups are at higher risk:
– Young children: Especially those under two years old.
– Elderly individuals: Due to weakened immunity.
– Immunocompromised patients: Such as those undergoing chemotherapy or living with chronic illnesses.
– Healthcare workers: Due to frequent exposure.
Preventive measures and treatment courses
Preventing hMPV involves basic hygiene practices: regular handwashing, avoiding close contact with sick individuals, and disinfecting surfaces. In healthcare settings, wearing masks and using gloves can reduce transmission risk. For those infected, isolation and symptomatic treatment remain key. Doctors emphasize the importance of monitoring symptoms and seeking timely medical intervention.
Comparison to COVID-19 times
The COVID-19 pandemic heightened global awareness of respiratory viruses, leading to improved hygiene and rapid vaccine development. However, hMPV highlights the need for continued vigilance against other pathogens. Unlike COVID-19, hMPV lacks a unified public health response, underscoring the importance of advancing research and healthcare infrastructure.
What we are thinking about it
Human Metapneumovirus may not have the global notoriety of COVID-19, but its impact is undeniable. From its silent spread to its severe effects on vulnerable populations, hMPV serves as a reminder of the ever-present threat of respiratory viruses. Addressing this challenge requires a combination of public awareness, medical innovation, and preventive strategies. As we have endured a post-COVID world, the lessons learned can guide our response to hMPV and similar pathogens, ensuring a healthier future for all.



